Novel Therapies for Preventing, Managing and Treating Obstructive Sleep Apnea and Snoring in Pediatric and Adult Patients
Sheats, R., Masse, J.-F., Levine, M., Aarab, G., Meira e Cruz, M., Simmons, M., Stauffer, J., Carstensen, S., Chiang, H., Galang-Boquiren, M. T., & Postol, K. (2024). Novel therapies for preventing, managing and treating obstructive sleep apnea and snoring in pediatric and adult patients. Journal of Dental Sleep Medicine, 11(2). https://doi.org/10.15331/jdsm.7332
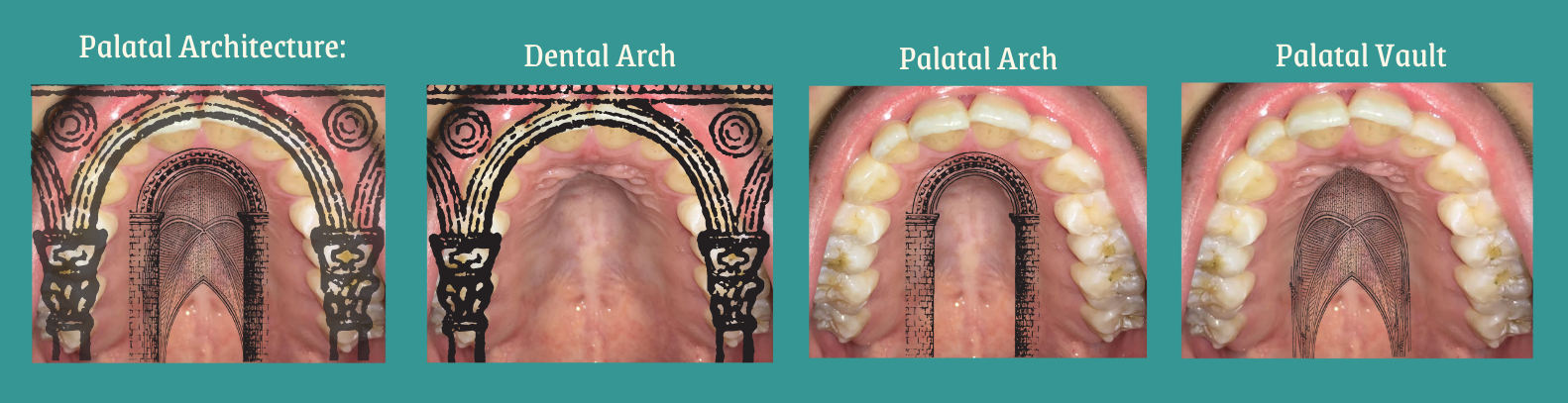
Form vs Function: What Follows What?
Zohara Nguyen, CCC-SLP, CPSP, QOM
"Form follows function" is a well-known phrase, but does it apply to orofacial growth and development? We discuss the "chicken or the egg" dilemma in the context of myo issues, stimulating orofacial myologists to recognize the interplay between Form and Function in their clients.
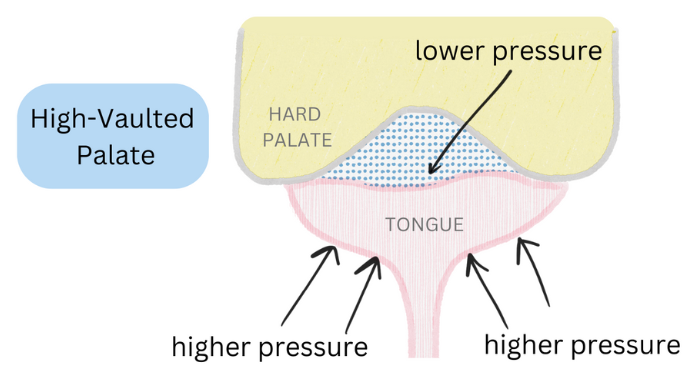
What is Lingual-Palatal Suction and When is it Compromised?
Zohara Nguyen, CCC-SLP, CPSP, QOM
Have you considered all of the necessary maneuvers to achieve Lingual-Palatal Suction or considered how it relates to the physics of a suction cup?
Labial Frenulae – Important Orthodontic Considerations
Robert Mason, DMD, PhD
When is the labial frenula problematic and what considerations indicate the need for a release?
More Myo Articles
The following papers are provided so that professionals can consider the various factors involved when making decisions about assessments and treatment for their clients. Neo-Health Services does not necessarily endorse everything included in the papers.
International Journal of Orofacial Myology and Myofunctional Therapy
All papers published in the IJOM are dedicated to the study and management of orofacial myofunctional disorders since 1975. They are openly available and can be searched in digital open-access format at the following link: ijom.iaom.com/
Bibliography
Afzelius-Alm A, Larsson E, Löfgren CG, Bishara SE.(2004). Factors that influence the proclination or retroclination of the lower incisors in children with prolonged thumb- sucking habits. Swed Dent J. 28(1):37-45.
Ballard, JL, et al (2002), Ankyloglossia: Assessment, Incidence, and Effect of Frenuloplasty on the breastfeeding dyad. Pediatrics 110;e63
Dimberg L, Bondemark L, Söderfeldt B, Lennartsson B. (2010). Prevalence of malocclusion traits and sucking habits among 3-year-old children. Swed Dent J. 34(1):35-42
Fernando, C. (1998). Tongue Tie from confusion to clarity. Sidney, Australia: Tandem Publications
Green, H, & Green, S. (1999), The Interrelationship of Wind Instrument Technique, Orthodontic Treatment, and Orofacial Myology. IJOM 25: 18-29
Green, S.(2009) Concomitant trichotillomania cessation and thumb-sucking elimination: of course, they're related...aren't they? IJOM Nov;35:55-73.
Hahn, V. & Hahn H. (1992), Efficacy of Oromyofunctional therapy. IJOM, 18, 22-23
Hanson, M.L. & Mason, R.M. (2003). Orofacial Myology: International Perspectives. Springfield, IL: Charles C. Thomas.
Hazelbaker, Alison ATLFF http://pediatrics.aappublications.org/content/110/5/e63/T1.expansion
Larsson E. (2001). Sucking, chewing, and feeding habits and the development of crossbite: a longitudinal study of girls from birth to 3 years of age. Angle Orthod. Apr;71(2):116-9.
Mason, R.M. (2011). Myths that persist about orofacial myology, IJOM, Vol 37:26-36. Mills, C.S (2012),History of the IAOM, IJOM, Nov.,Vol.37:5-25
Mukai S, Mukai C, Asaoka K. (1993) Congenital Ankyloglossia with deviation of the epiglottis and larynx. Ann Otolaryngol;102: 620-4
Niedenthal, Paula M., Augustinova, Maria, Rychlowska, Droit-Volet, Magdalena Sylvie, Zinner, Leah, Knafo ,Ariel & Brauer, Markus (2012): Negative Relations Between Pacifier Use and Emotional Competence, Basic and Applied SocialPsychology, 34:5, 387-39
Proffit, W.R., Fields, Jr,H.W. & Sarver, D.M.(2012), Contemporary Orthodontics, 5th Edition, St. Louis, MO, C.V.Mosby
Sexton S, Natale R. (2009). Risks and benefits of pacifiers, Am Fam Physician. Apr 15;79(8):681-5.
Tillmann, B.N. (2007). Atlas of Human Anatomy. Mud Puddle Books, Inc., New York, NY. Van Norman, R.A. (1999). Helping the Thumb-Sucking Child. Avery Publishing Group, Garden City Park, NY.
Van Norman, R. (1997). Digit sucking: a review of the literature, clinical observations and treatment recommendations. International Journal of Orofacial Myology. 23(1). 14-34
Warren JJ, Bishara SE, Steinbock KL, et al (2001). Effects of oral habits' duration on dental characteristics in the primary dentition. J Am Dent Assoc. Dec;132(12):1685-93; quiz 1726.
Weiss, TM, Atanasov, S & Calhoun, KH, (2005), The association of tongue scalloping with obstructive sleep apnea and related sleep pathology, Otolaryngol Head Neck Surg. Dec;133(6):966-71, Department of Otolaryngology, Southern Illinois University, USA.