What is Lingual-Palatal Suction and When is it Compromised?
Published: August 22, 2023
We all recognize the importance of lingual-palatal suction (LPS) for our clients, but have you considered all of the necessary maneuvers to achieve this? Have you considered how it relates to the physics of a suction cup? Take a tiny sip of water and trap it to your palate while holding your lips and mouth open. If you can do this without spillage, you are demonstrating LPS, one of our most important goals in treatment.
What is the physics of lingual-palatal suction?
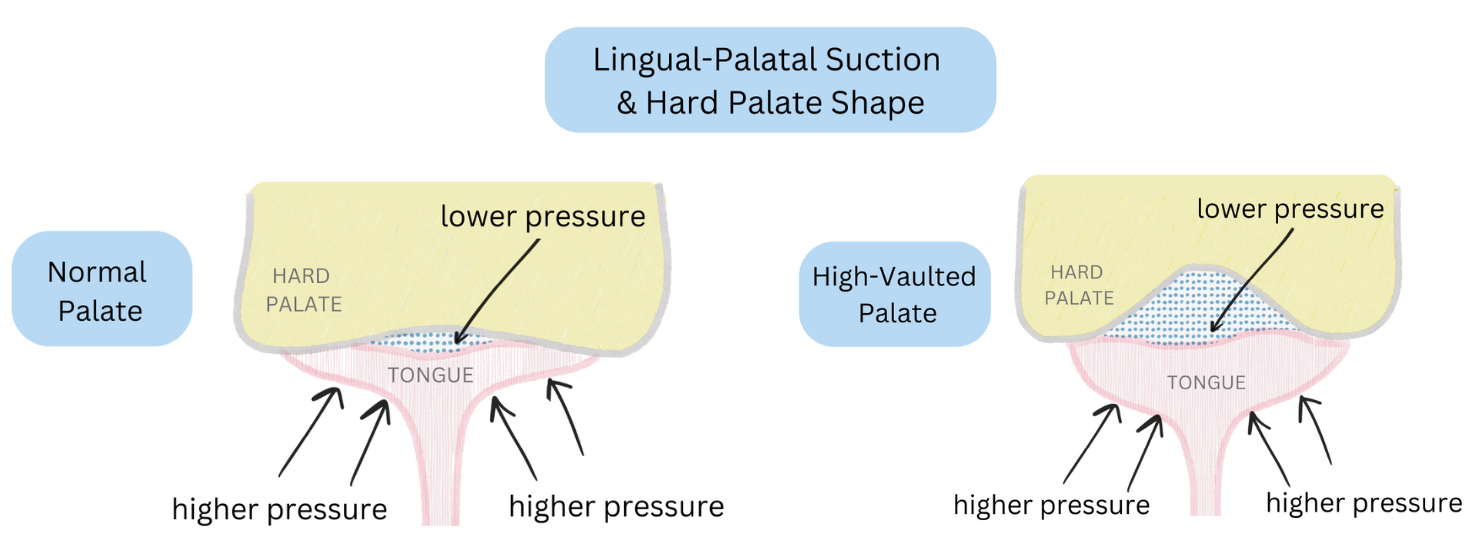
As the tongue is pressed flat against the palate and air is forced out, negative pressure (suction) occurs as a result of low pressure air in the chamber between the dorsum of the tongue and the palate. For suction to occur, the atmospheric air pressure outside of the chamber (the rest of the mouth) is higher than the air pressure inside of the chamber. Since atmospheric pressure tries to equalize by moving high pressure towards areas of lower pressure, the underside of the tongue pushes towards the palate, allowing it to maintain lingual suction once some air is squeezed out. Of course a seal around the chamber reinforces the LPS. Not only do the borders of the tongue have to seal to the palate, but the posterior of the tongue contacts the soft palate to create a posterior seal. Saliva also contributes to lingual suction, since it creates a tighter seal around these borders (it’s a known fact that suction cups work even better when you wet them)!
Altering lingual-palatal suction and the physics of “tongue clicks”.
Did you know that we can alter LPS at will? We can do this by creating a light lingual suction (the underside of the tongue looks soft), or we can initiate a forceful lingual suction (creating dark caves under our tongue). By lifting the posterior of the tongue towards the palate, we reduce the lingual-palatal pressure and enhance the suction created. When we break this suction by pulling the tongue away from the palate, there is a sudden change in air pressure as the air equalizes. The sudden change in pressure from low to higher atmospheric pressure creates a pressure wave which is interpreted as a “click” or a “giddy-up” sound.
Which oral issues can affect lingual suction?
There are a few variations in palatal presentations that should be considered in myo because they can influence lingual suction skills. Hence, clients with these presentations should be maximized, with a likelihood of treatment modifications.
- A high vaulted hard palate - Lingual suction might be weaker since the vault of the palate makes it physically difficult to force air out to an appropriately low pressure for adequate suction. You might notice that individuals with high palatal vaults often move their tongue tip into the vault or jam the middle of their tongue up into the vault. This reduces the air pressure in the chamber to achieve a stronger lingual suction.
- Narrow dental and palatal arches - For those with narrow dental and palatal arches, issues might arise when attempting to create LPS, due to the lack of space. This can result in overflow onto the occlusal surfaces of the teeth. Overflow forms gaps in the seal and opportunities for air to escape.
- Repaired cleft palate - Lingual suction might not be successful due to a lack of complete posterior tongue contact with a repaired soft palate. As stated above, difficulties might also occur with a narrow, V-shaped palate post-repair or if there is a tiny fistula post-repair.
- Palatal torus - Depending on the size of the torus, it might occupy too much palatal space. Some tori are so large that they could interfere with the “flat” suction of the tongue to the palate and its ability to be maintained.
From the above examples, we realize there are many components and considerations to be taken into account when planning treatment for individuals with differences in their palatal structures. Understanding the physics helps us to deeply understand the tasks that clients are being asked to do in treatment, and the modifications needed for long-term progress to “stick”.